I learned that other professions along with mine need to get together...and try to make a plan to help the patient.
Respiratory Therapy Student
I learned that other professions along with mine need to get together...and try to make a plan to help the patient.
Respiratory Therapy Student
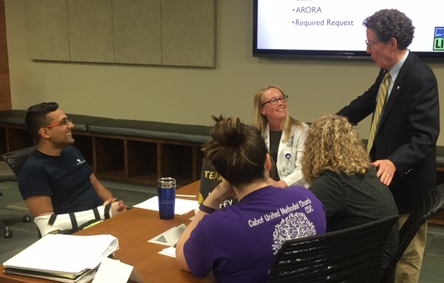
At the University of Arkansas for Medical Sciences (UAMS), the Office of Interprofessional Education (IPE) operates within the UAMS Division of Academic Affairs and coordinates an interprofessional curriculum that is a graduation requirement for all UAMS students in the Colleges of Medicine, Pharmacy, Nursing, Health Professions, Public Health and the Graduate School. The UAMS focus on interprofessional education and collaborative practice aligns with the Triple Aim approach to health care performance.
With strong support from the UAMS Chancellor, the Council of Deans and the Vice Chancellor’s Advisory Committee, the Office of Interprofessional Education was formed in 2013. A Director and a 12-member steering committee with representation from each of the UAMS colleges and the graduate school were appointed. The UAMS IPE Triple Aim Curriculum Framework was developed by the committee and approved through each college and programs’ curriculum oversight process. Within the approved curriculum framework, students complete seven core activities aligned with professional development in novice (exposure), intermediate (immersion), and advanced (competence) levels. Core activities include:
To date, in the 2016-2017 academic year, 23 events have been delivered to more than 1600 enrolled students.
The infrastructure for the IPE program has grown to include 3 directors and 5 “pillar teams” composed of more than 100 faculty, staff, and patient/family educators that lead initiatives for (1) Curriculum Implementation and Evaluation, (2) Development (fundraising), (3) Scholarship and Research, (4) Faculty Development, and (5) Collaborative Practice.
Currently, over 30 discrete IPE curriculum events are in place for students. Learning outcomes related to content-specific learning objectives, patient- and family-centered care skills, and interprofessional practice outcomes are tracked longitudinally. A standardized rubric is used to assess qualitative reflections from students that are used to evaluate knowledge of self (own profession), interprofessional team (other professions), and context (Triple Aim).
More than 100 faculty members have been trained; quantitative and qualitative metrics are used in evaluation of faculty development programming. A process for certification of IPE facilitators is in place. Faculty may be recognized as Master Facilitators if they are certified in 3 different types of IPE activities.
Kathryn Neill, Pharm.D., Director of Interprofessional Administrative and Curricular Affairs, identifies several factors as key in the program’s success:
She offers the following advice to other institutions that are developing an IPE curriculum, involving patients/families as educators:
In the UAMS IPE program, patient/family educators are involved in all four elements: