Shared Principles of Primary Care
Developed by a broad group of stakeholders, led by PCPCC, the Shared Principles describe seven important attributes of advanced primary care. They are designed to help move the United States toward a future of health care that is person- and family-centered, team based, and aligned with the community. Realizing this ideal future of primary care requires a common vision among all stakeholders, with the goal of achieving better health, better care, and lower costs. The seven attributes are:
- Person and Family Centered
- Continuous
- Comprehensive and Equitable
- Team-based and Collaborative
- Coordinated and Integrated
- Accessible
- High-Value
Person and Family Engagement (PFE) Performance Metrics
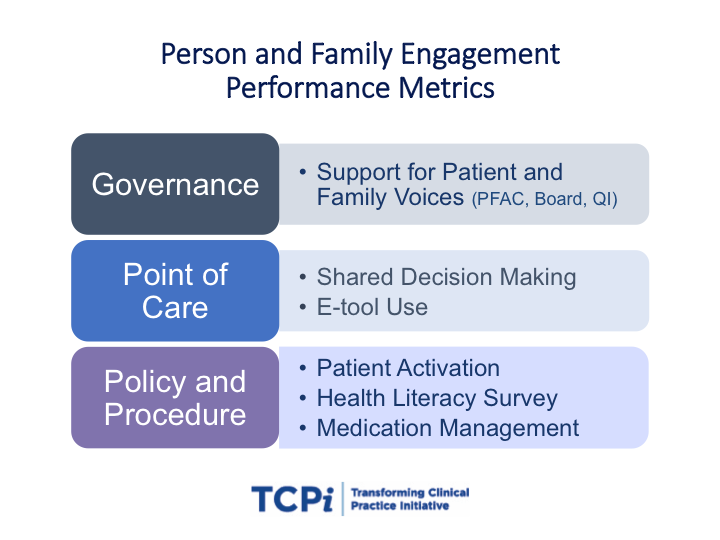
Six person and family (PFE) performance metrics cover three fundamental domains of best PFE practice, Point of Care, Policy & Procedure, Governance. The metrics address key strategies that can be adopted by practices to engage patients and families as partners in decision-making. The metrics address different aspects of engagement.
6 Steps to Creating a Culture of Person and Family Engagement in Health Care
This toolkit is designed for healthcare practices participating in TCPI, but will be of value to any practice seeking strategies to improve person and family engagement. It provides guidance on creating a practice culture that emphasizes and incorporates the patient and family perspective in every aspect of care, to ultimately improve quality of care.
 Advancing the Practice of Patient- and Family-Centered Care in Primary and Other Ambulatory Settings: How to Get Started
Advancing the Practice of Patient- and Family-Centered Care in Primary and Other Ambulatory Settings: How to Get Started
Within the framework of patient-and family-centered care, this IPFCC document outlines steps a primary care clinic or ambulatory practice can take to begin to create partnerships with patients and families, and offers practical suggestions for getting started.
Individual and Family Engagement in the Medicaid Population: Emerging Best Practices and Recommendations
This IPFCC issue brief outlines best practices and suggested recommendations and strategies to support enhanced individual and family engagement efforts by Medicaid agencies, their staff, and organizations serving these populations.
Toolkit to Engage High-Risk Patients in Safe Transitions Across Ambulatory Settings
Patients who transition from one ambulatory care clinician to another are vulnerable to patient safety errors. To address this need, the Health Research & Educational Trust (HRET) adapted select, evidence-based patient and care partner-centered acute care discharge tools to create a toolkit specifically for use in the ambulatory care setting. The toolkit is designed to help staff actively engage patients and their care partners to prevent errors during transitions of care and includes a detailed implementation guide, a pre-intervention assessment, patient appointment aide, checklist for clinicians, and an educational video.